Voices and adversity
Where people live, whether they are struggling financially, and access to educational and other opportunities have also been linked to voice-hearing in cases where people have a diagnosis of psychosis. For example, found that and can increase a person’s risk of developing psychosis, as can living in a city as opposed to a rural area. Inequality is also a contributing factor. Poor people living in neighbourhoods where richer people also live tend to have a greater risk of developing psychotic experiences than those living in neighbourhoods where most people have a similar income.
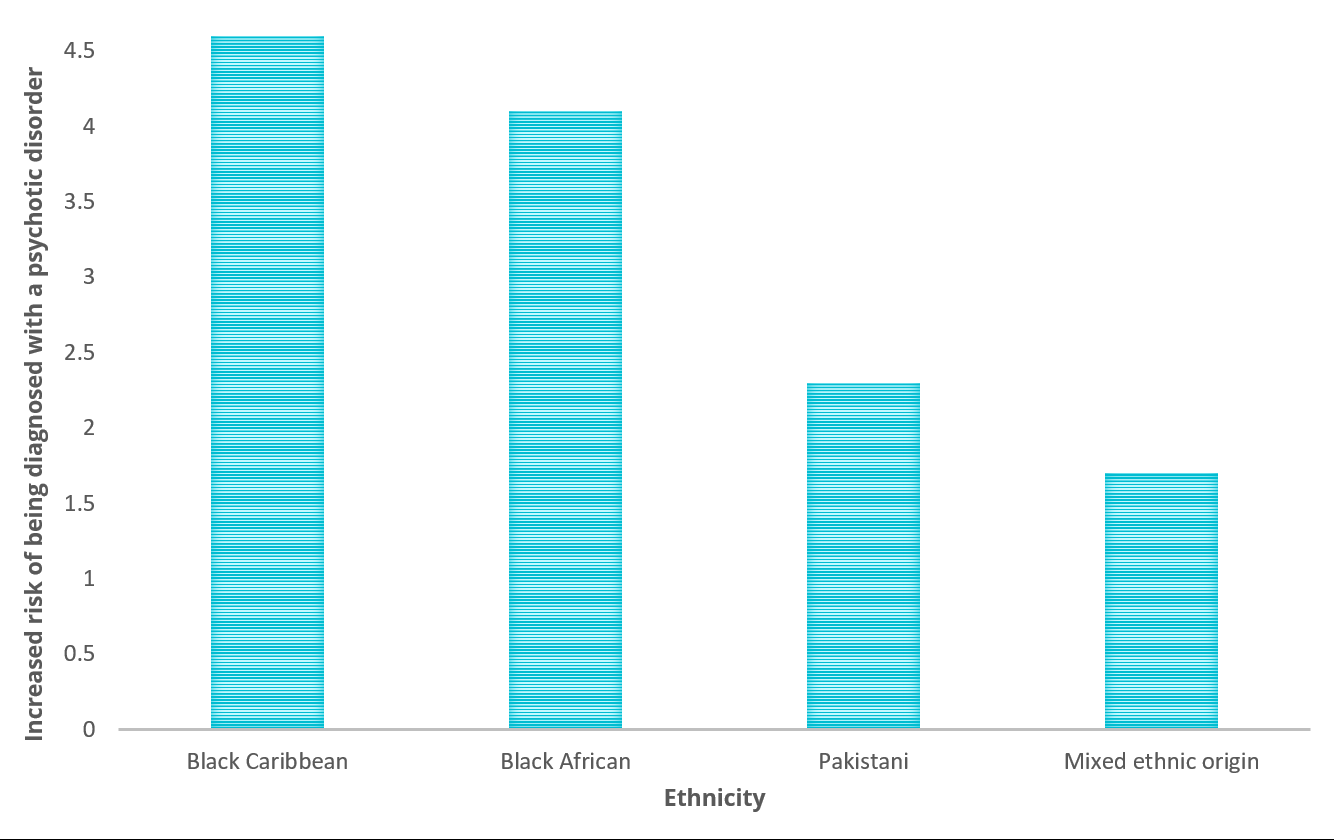
People from minority ethnic groups living in the UK are much more likely than white British people to be diagnosed with schizophrenia or other psychotic disorders. This is true regardless of whether they have been born in the UK or have migrated here from other countries. Exactly why this happens is unclear, but , deprivation, , every-day and are known to contribute to the problem.
Ethnicity and risk of developing psychosis
But while there seems to be a clear link between having a difficult life, social exclusion, racism and being diagnosed with schizophrenia or psychosis, less work has been done specifically on the relation between these factors and hearing voices. It does seem to be the case, though, that the more difficulties and dangers an individual is exposed to, the higher their likelihood of developing unusual experiences and beliefs, including hearing voices. have suggested that, in certain African American communities at least, high rates of abuse, poverty, gang violence, drug use and repeated experience of racism are reflected in the nature of the voices people experience – what they are like, what they say, and the meanings people attribute to them.
What causes psychosis?
When we come into contact with services, those of us from BME backgrounds, and especially young black men, are more likely than others to receive a diagnosis of schizophrenia, even if the problems we are experiencing are much the same. We are also more likely to be detained (‘sectioned’), subjected to solitary confinement (‘seclusion’), medicated against our will, and given higher doses. This difference appears to be the result of misunderstanding, discrimination and stereotyping within services. Most people assume that racism refers to people being personally racist – for example, engaging in overtly and explicitly racist verbal abuse or actively treating people differently because of their ethnicity. However, a series of government inquiries have identified that, within institutions like the police or health service, people from black and minority ethnic backgrounds can end up being treated differently even if individual members of those institutions do not individually act in this way: this is known as institutional racism … As a result of this institutional racism people are also less likely to seek help early, and this can lead to a vicious circle.
Understanding Psychosis and Schizophrenia (Revised Edition, Section 6)
Find out more
Read
Nicola Davis (2017). Risk of psychotic disorders up to five times greater for people from ethnic minorities – UK study finds. The Guardian.
Vaughan Bell (2016). The Mystery of Urban Psychosis. The Atlantic.
Jason McIntyre and Richard Bentall (2017). Immigrants suffer higher rates of psychosis – here’s how to start helping them. The Conversation.
James B. Kirkbride (2017). Migration and Psychosis: Our smoking lung?. Wiley Online Library.
Jingyi Wang (2018). Loneliness in psychosis and related psychological and social factors’. The Mental Elf.
James B. Kirkbride et al (2017). Ethnic minority status, age-at-immigration, and psychosis risk in rural environments. Schizophrenia Bulletin.
Cherise Rosen et al. (2017). Exploring the Intersections of Trauma, Structural Adversity, and Psychosis among a Primarily African-American Sample: A Mixed-Methods Analysis. Frontiers in Psychiatry 8(8).